We are all witnessing the COVID-19 pandemic ushering in a new normal for the world – businesses are closed across the country and the provinces are releasing individualized action plans for re-opening in phases. These plans are aiming to make businesses safer for everyone and reduce the potential for spread of infectious diseases. Developing these plans is particularly challenging for medical clinics and dental offices where at-risk individuals are often present within close quarters – the normal precautionary measures are difficult to implement without limiting productivity.
The most prominent measure at the forefront of the public eye is social distancing – to reduce the transmission of the virus via droplets from coughing, sneezing, talking, and breathing we are being encouraged to maintain a 2 meter [6 ft] distance away from each other. The public has bought into these measures and has collectively been successful at flattening the curve. Social distancing within medical and dental offices, however, is often not possible, forcing these offices to limit the number of patients able to safely enter the space.
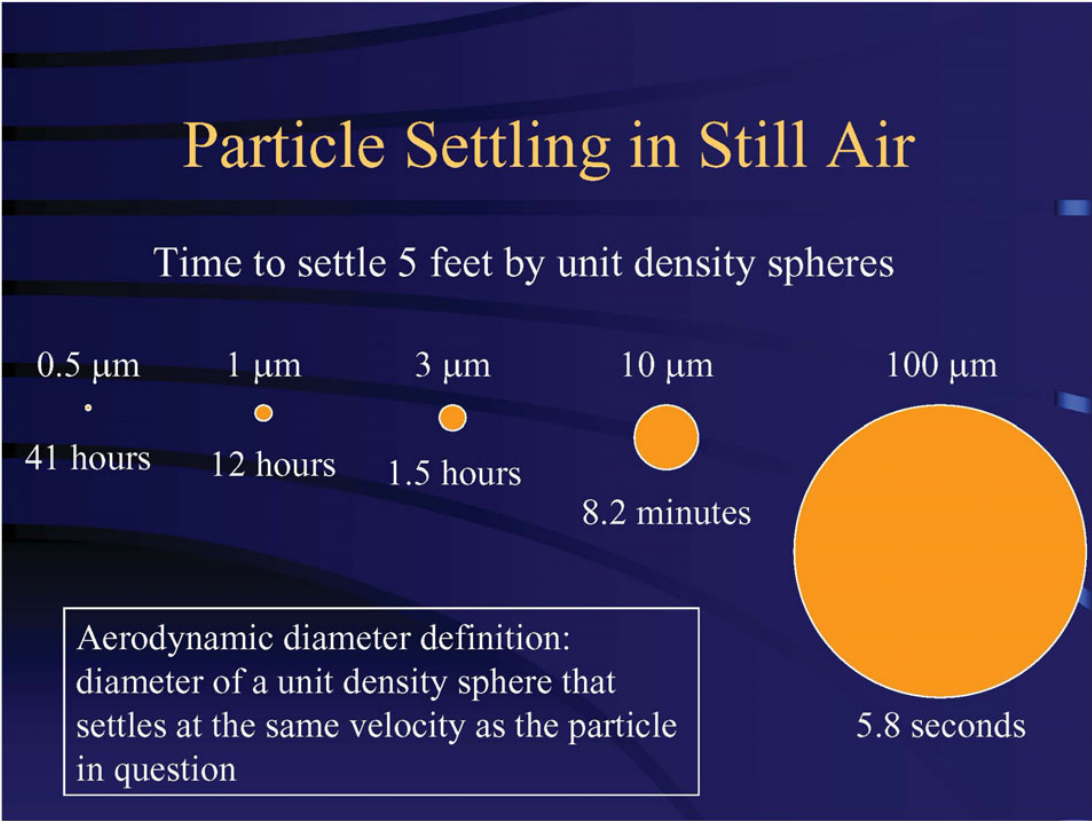
There is also evidence emerging that smaller droplets are able to travel much larger distances that social distancing cannot guard against. Droplets ranging from 5 to 10 μm in diameter are generally only an airborne threat within 2 meters [6 ft] of their source – droplets smaller than 5 μm on the other hand are much lighter and have the potential to remain airborne for longer periods of time during which they can be transported large distances by building ventilation systems. For context, the diameter of COVID-19 ranges from 0.06 to 0.14 μm.
Figure 1 – Particle Settling in Still Air Source: [1] (ASHRAE, 2020)
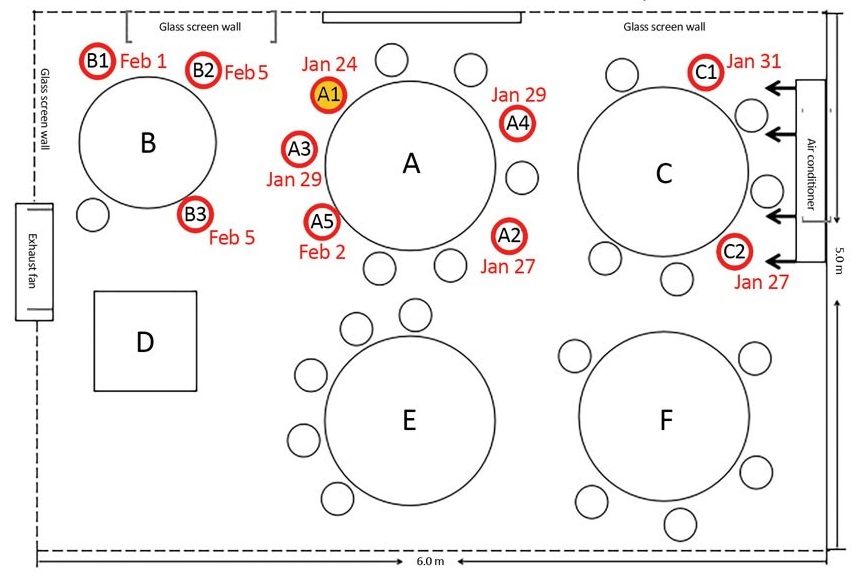
Furthermore, a case study has emerged showing that airborne transmission influenced by the air conditioning system led to the spread of the virus in a restaurant in Guangzhou, China – customers seated at distances greater than 2 meters away from the suspected source contracted the disease [1]. There are also hypotheses suggesting that airborne transmission of the disease via the ventilation system occurred aboard cruise ships that experienced mass infection. The University of Alberta is among the research institutes currently further investigating the role HVAC systems play in the airborne transmission of SARS-CoV-2 and expect results to be available in Summer 2021 [2].
Figure 2 – Sketch showing restaurant and air conditioning airflow at restaurant in Guangzhou, China. Source [2]
In the meantime, the American Society of Heating, Refrigeration, and Air Conditioning Engineers (ASHRAE), has outright stated that transmission of the virus through the air is sufficiently likely and that airborne exposure to the virus should be controlled – changes to the operation of the HVAC systems can reduce airborne exposures [3]. The World Health Organization (WHO) on the other hand, acknowledges airborne transmission as a potential mode of dissemination but is refusing to make any further recommendation until a solidified peer reviewed study is released [4]. Despite the lack of consensus on the modes of disease transmission, there appears to be a very real risk of an infected individual entering a medical office and indirectly transmitting the disease to the patient entering the office for the subsequent visit or even to the patient in the neighboring exam room via the ventilation system.
To combat this risk, the Saskatchewan Health Authority has released their plans for the re-opening of dental offices which includes minimum settling times after aerosol generating medical procedures – if ventilation is not sufficient, there must be a scheduled downtime of 2 hours between procedures [5]. This is a significant period of non-productive time. We have not yet seen similar requirements released by the province of BC – but we as mechanical engineers feel we can offer some simple solutions to improve the ventilation systems within these buildings to reduce potential downtime and also make them a safer space for patients and employees alike.
We can do so by taking the following approaches:
- Increase Volume of Outside Air introduced to Space
- This methodology is known as dilution ventilation whereby an increased amount of fresh outside air is brought into a space to dilute the infected air. Many older buildings have an insufficient amount of fresh air being brought in.
- Increasing the supply air to a room is increasing the ACH (Air Changes per Hour) which is an industry term for how many times the air within a given room changes per hour. The Saskatchewan Health Authority has determined that a room with 20 ACH will take 21 minutes to reduce airborne contaminants by 99.9%. [6]
- Increase Volume of Air Exhausted from Space
- This methodology is known as displacement ventilation whereby the stale, and potentially infected, room air is exhausted to the outside rather than being recirculated
- Exhausting inside air rather than recirculating it, although less energy efficient will improve air quality.
- Enhance Filtration
- Filtration of recirculating inside air or even fresh outside air can trap small particles and contaminated aerosols
- A NASA conducted study found that HEPA-rated media is capable of removing virtually 100% of particulates including ultrafine particles less than 0.01 μm in diameter which would include viruses.[7]
TAG Engineering is currently working with owners and contractors on all of our current and future builds to incorporate these improved safety measures. We are also offering our services to conduct individualized audits for owners looking to boost the ventilation health of their existing spaces – we can inspect your current ventilation systems and give you an assessment of how it is performing. We can then offer you the best solution or combination of solutions to make your space safer for your patients, your staff, and yourself. Please do not hesitate to reach out to further discuss what we are able to offer.
We here at TAG are keeping our eyes and ears open for new developments related to keeping ourselves safe. For now, we must all continue to heed our instructions from our Public Health Officers and continue to regularly wash our hands, maintain our social distance, and avoid large crowded areas. Together we can stomp out this pandemic!
References
| [1] | J. Lu, J. Gu, K. Li, C. Xu, W. Su, Z. Lai, D. Zhou, C. Yu, B. Xu and Z. Yang, “COVID-19 Outbreak Associated with Air Conditioning in Restaurant, Guangzhou, China, 2020,” Emerging Infectious Diseases, vol. 26, no. 7, 2020. |
| [2] | Canadian Institutes of Health Research, “Government of Canada funds 49 additional COVID-19 research projects – Details of the funded projects” 2 April 2020. |
| [3] | ASHRAE, “ASHRAE Position Document on Infectious Aerosols” 14 April 2020. |
| [4] | World Health Organization, “Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations” 29 March 2020. |
| [5] | Saskatchewan Health Authority, “COVID-19 PPE Rapid Update” 23 April 2020. |
| [6] | Saskatchewan Health Authority, “NOVEL CORONAVIRUS (COVID-19): Interim Infection Prevention and Control” 27 March 2020. |
| [7] | National Aeronautics and Space Administration, “Submicron and Nanoparticulate Matter” 16 May 2016. |

Recent Comments